Dundee Health & Social Care Partnership’s Psychiatry of Old Age service includes In-patient Services, Post Diagnostic Support Team (PDST), Community Teams (CMHTOP) and the Care Home Team (CHT). It is located in the Kingsway Care Centre in Dundee.
These teams can follow the patient in to and out of hospital where appropriate, to offer further care and support. Within these teams, there are a range of professionals from Nursing, Pharmacy, Medical, Allied Health Professionals, Social Work and Clinical Psychology. This means that staff with specialist skills from different areas can see patients more easily. Length of patient admission ranges from a couple of weeks through to longer admissions depending on the complexity of their presentation or the waiting lists for recommended care. The average admission time is 6-12 weeks.
The Occupational Therapy service is integral to all of the teams and play a key role in treatment and discharge planning. This case study describes how the Occupational Therapy Team uses the What Matters To You? (WMTY) approach during recovery group sessions and 121 ‘values session’ with the patient
HOW THE ‘WMTY’ APPROACH IS USED
When a patient is admitted, an occupational therapist carries out an initial assessment. This is a collaborative process in which the Occupational Therapy treatment and assessment plan is agreed.
These sessions and the associated responses are used to work with the patients to develop a person centred action plan for recovery, which can require joint working with other members of the multidisciplinary team. The recovery programme is led by the occupational therapist and a nurse key worker with additional support from Activity Worker or Health care assistants as appropriate. With agreement of the participants, we can also offer work shadow opportunities.
WRAP (Wellness Recovery Action Plan) is a self management tool designed to help patients take control of their own health and wellbeing. It recognises that they are the expert in their own experience and there are no limits to recovery. It helps patients to identify their own wellness tools and which coping strategies are helpful or unhelpful, thus allowing them to have ownership of their every day mental health issues. Patients can use recovery plans, every day, weekly, monthly or yearly. It is a truly person centred tool designed for and used by them.
- Development of recovery plans
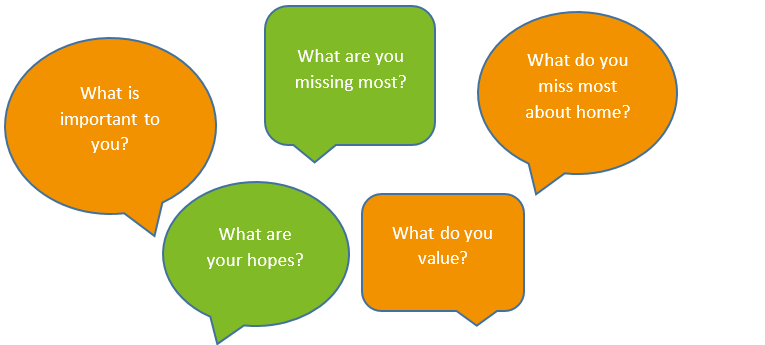
During a 121 ‘values session’ WMTY questions are used, please see speech bubbles below. WMTY type questions fit perfectly within the context of understanding what is important to patients when developing their recovery plan since it includes, for example:
- support that is available to them, including advocacy
- the patient’s personal responsibilities
- education about mental health in general, and more specifically about their condition
- building self-awareness, and
- how the patient can self-manage their condition.
Finding out what the patient misses from home and who or what the patient values helps both staff and patients put into place things that will make their hospital stay more comfortable. Many of these discussions lead to this being put into place before they are discharged.
One patient was asked ‘what are you missing most about home?’ she said she missed her favourite shoes. Following this, the Occupational Therapist took the patient home to collect her shoes. This gave us consent to carry out an Occupational Therapy home assessment and gain insight in to the importance of walking to them. It also led to an open discussion about the triggers to the person’s admission, being able to provide education about early warning signs and discover how important walking was in their wellness toolbox. Walking was then built in to their daily maintenance plan and they were supported to attend the Occupational Therapy walking group, which has run once weekly for several years. This helped to alleviate some anxieties about their physical health, build up their walking tolerance as well as increasing their social interactions. As part of the ongoing Occupational Therapy post discharge follow up, information and support to join a community walking group was also put in place through social prescribing.
1. Recovery group session
Recovery group sessions are held where patients are encouraged to discuss values as a group, using simple WMTY questions such as:
This foundation to recovery work establishes shared values as well as identifying individual’s hopes and this can be used to help the service deliver a person centred recovery process. Patients will interact and find similarities and differences in what they value.
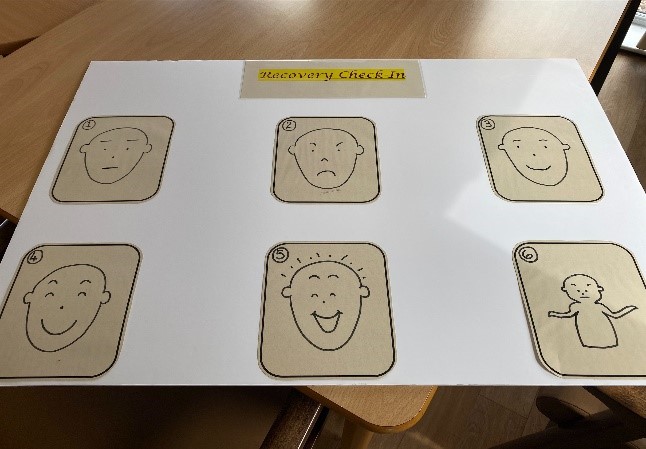
Through the use of a simple questionnaire – based on the Care Measure facial expression visual aid, patients are presented with visual images and asked to pick one and give a word to describe how they feel. Staff ask patients to complete this as a ‘check-in and check-out’ process for every group session, but if an individual finds this difficult, it can be done on an individual basis.
Staff recognise it is important to get clarity about why a patient has selected a face. Some people may always select the same face but when asked for a word, this can show a difference in how they feel. For example, a patient may select a sad face when they arrive for a group session, and again before they leave, but the word they use shows they feel some difference. Using this method helps staff to evaluate the difference the session has made to people and identify any changes or improvements they can make. It can also be used to show a patient their responses over a period of time to help them see they have improved, something that can be difficult for the patient to identify in themselves or that they are having difficulty accurately self-reporting or self-monitoring their mood. Often peers will offer the feedback to the individual giving examples of things they have observed which indicate an improvement in their mental health.
For example one lady said to another patient ‘Of course you are not a bad person or useless. You are very caring. You brought me in my favourite marmalade and even helped me open the jar’. It is often the feedback from peers, which is valued and accepted more than any staff feedback.
People with mental health issues can find it difficult to express themselves or make decisions, common to the clinical features of depression. Peer support within the community of the ward encourages peer interactions wherever possible, and promotes a sense of belonging. Peer observation is relevant and over longer periods so can be as good as or better than that of staff, who see someone in controlled and/or short sessions. Patients do not want staff to be their only support, they want to feel normal and have normal interactions. It is therefore important to know what matters to them and they can seek out individuals who share the same values.
KEY BENEFITS
- Asking people about what matters to them helps us to deliver person centred care and establish rapport at an early stage in the admission.
- Through using a variety of questions to address values and recovery, we have a list of topics the patients identified as being something that matters to them. These can then be addressed through the recovery groups.
- For patients who find it difficult to communicate verbally, the use of visual aids helps us to identify what is important to that person.
- While these patients are acutely unwell, they are not excluded from being asked their opinions. They are able to offer valuable insights in to how the services work for them, how services are perceived and what matters to them at the time of treatment.
- Sometimes patients come in 2-3 times in a year and can give different information as their understanding widens and they become more self-aware.
One in-patient said they used their recovery plan and recognised that their early warning sign was loss of interest in meal preparation, which came before loss of appetite. They contacted their Community Mental Health Nurse and were readmitted as they had also deteriorated re medication compliance, food, and fluid intake. His inclusion in the recovery groups has been very helpful for his peers and himself. He is a strong advocate for taking part in recovery and how important identifying what mattered to him was. He felt empowered by ultimately being able to use his recovery plan. In doing so, he recognises that what he truly values is being able to/learning to self-manage and that he values the importance of mental health. Furthermore and altogether, more powerful is that by doing so he is now valuing his life and it is a privilege to be a part of that transformative process.
KEY CHALLENGES
- Ensuring we have a group of patients who are at the same stage in their recovery so they can work together and share the same level of comprehension of topics covered.
- A core principle of recovery is the completion of homework and participation in group sessions, but this is entirely voluntary. Patients don’t need to share in the group and indeed that is one of the basic rules ‘share only what you want to share and are comfortable to share’, although they are encouraged to do so.
Contact details:
Donna Mackintosh
Kingsway Care Centre
Kings Cross Road
Dundee
DD2 3PT Email Donna.Mackintosh2@nhs.scot